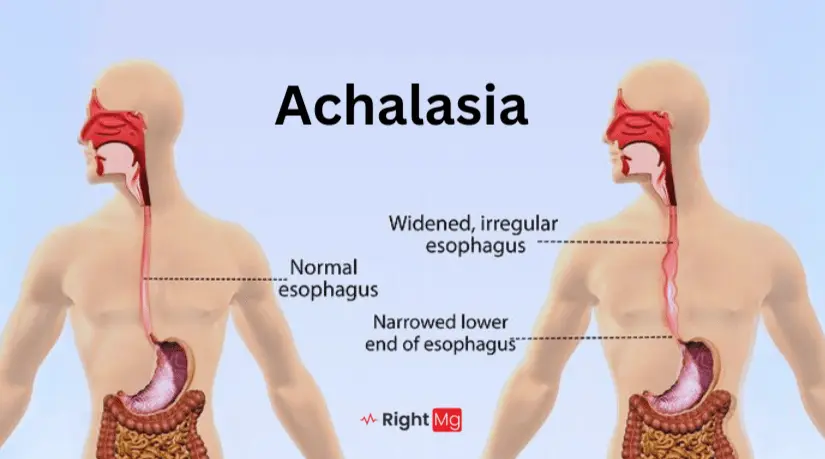
Achalasia is a rare esophageal disorder that affects the ability of the esophagus to move food toward the stomach. The esophagus is the muscular tube that carries food and liquids from the mouth to the stomach. In people with achalasia, the muscles of the esophagus don’t work properly, and the lower esophageal sphincter (LES) fails to relax properly, making it difficult for food and liquids to pass into the stomach. This can lead to a variety of symptoms and complications if left untreated.
Understanding the Esophageal Mechanism
Swallowing is a coordinated effort involving muscles and nerves. During a swallow, the upper esophageal sphincter relaxes, allowing food to enter the esophagus. The esophageal body then propels food downwards through peristalsis, a wave-like muscular contraction. Finally, the lower esophageal sphincter (LES) relaxes to permit food passage into the stomach.
The Breakdown in Achalasia Cardia
In achalasia cardia, the normal esophageal function goes away. The key culprit is the degeneration of nerve cells within the esophageal wall. This disrupts the messaging system, leading to:
- Impaired Peristalsis: The coordinated muscular contractions in the esophageal body are absent or weak.
- LES Dysfunction: The LES, instead of relaxing with a swallow, remains tightened, creating a blockage at the entrance to the stomach.
Types
Achalasia can be classified into different types based on the pattern of esophageal motility and the degree of sphincter relaxation. The primary types include:
- Type I (Classic Achalasia): Characterized by minimal or no esophageal peristalsis and a completely non-relaxing LES.
- Type II (Achalasia with Compression): Shows pan-esophageal pressurization where the entire esophagus contracts together rather than in a wave.
- Type III (Spastic Achalasia): Defined by abnormal, spastic contractions of the esophagus and a partially relaxing LES.
Symptoms
The symptoms of achalasia can develop slowly and may be mistaken for other gastrointestinal issues. Common symptoms include:
- Dysphagia: Difficulty swallowing, often for both solids and liquids.
- Regurgitation: Backflow of undigested food or liquids from the esophagus into the mouth.
- Chest Pain: Discomfort or pain behind the breastbone, which can be severe.
- Weight Loss: Unintentional weight loss due to difficulty eating.
- Heartburn: Although less common, some people may experience heartburn.
- Coughing or Choking: Especially during sleep, due to regurgitation of food.
Causes
The exact cause of achalasia is unknown, but it is believed to involve a combination of genetic, autoimmune, and environmental factors. Potential causes include:
- Nerve Degeneration: Loss of nerve cells in the esophagus and LES.
- Genetic Mutations: Rare genetic mutations may predispose individuals to develop achalasia.
- Autoimmune Response: The body’s immune system mistakenly attacks the nerve cells in the esophagus.
Risks
Several factors may increase the risk of developing achalasia, including:
- Age: Achalasia is most commonly diagnosed in individuals between 25 and 60 years old.
- Genetics: A family history of achalasia or other autoimmune disorders may increase the risk.
- Viral Infections: Some studies suggest that viral infections may trigger an autoimmune response leading to achalasia.
Diagnosis
Diagnosing achalasia typically involves a combination of tests and procedures, including:
- Barium Swallow: A special X-ray test where the patient drinks a barium solution to visualize and assess the shape and movement of the esophagus.
- Esophageal Manometry: Measures the rhythmic muscle contractions of the esophagus and the function of the LES.High-Resolution Manometry is The gold-standard test that measures esophageal pressure changes during swallows.
- Upper Endoscopy: A flexible tube with a camera is used to examine the inside of the esophagus and upper portion of stomach.
- Imaging Tests: Such as chest X-ray or CT scan to look for abnormalities.
Treatment
The goal of achalasia cardia treatment is to reduce the pressure of the LES and facilitate food passage. The choice of treatment depends on various factors, including patient health and disease severity. Treatment options include:
Pneumatic Dilation: A balloon is inflated within the LES to tear some muscle fibers and decrease pressure.
Peroral Endoscopic Myotomy (POEM): A minimally invasive procedure where a small incision is made in the LES muscle using an endoscope.
Laparoscopic Heller Myotomy: Surgical intervention involving a similar muscle incision in the LES, performed through laparoscopy. Cutting the muscles at the LES to allow easier passage of food.
Medications: Such as nitrates or calcium channel blockers to relax the LES.
Botox Injections: Temporary treatment that relaxes the LES muscles.
Natural Remedies
While natural remedies cannot cure condition, they may help manage symptoms. Some natural approaches include:
- Dietary Changes: Eating smaller, more frequent meals and avoiding foods that trigger symptoms.
- Hydration: Drinking plenty of water to help pass food through the esophagus.
- Positioning: Eating while sitting upright and staying upright for at least an hour after eating.
- Herbal Remedies: Some people find relief with herbal remedies like peppermint oil, which can relax the LES.
In Children
Achalasia is rare in children, but when it occurs, it presents unique challenges. Symptoms in children may include:
- Vomiting
- Failure to thrive
- Recurrent pneumonia due to aspiration
Diagnosis and treatment are similar to those in adults, with a focus on minimally invasive procedures to preserve growth and development.
In Teens
Teenagers with condition may experience:
- Difficulty swallowing
- Regurgitation of food
- Weight loss
- Chest pain
Treatment in teens often involves a combination of medications, endoscopic procedures, and surgery, tailored to the individual’s needs.
In Adults
Adults with achalasia typically present with:
- Dysphagia
- Regurgitation
- Chest pain
- Weight loss
Management in adults includes a range of options from lifestyle changes and medications to surgical interventions, depending on the severity of symptoms.
In Pregnancy
Achalasia can complicate pregnancy due to the increased pressure on the abdomen. Pregnant women may experience worsening symptoms, and treatment must be carefully managed to avoid harm to the fetus. Options include dietary modifications, medications considered safe during pregnancy, and, in severe cases, surgical intervention after delivery.
Home Remedies
In addition to medical treatment, some home remedies can help manage symptoms:
- Warm Liquids: Drinking warm liquids can help relax the esophagus.
- Chewing Thoroughly: Chewing food thoroughly before swallowing can make it easier to pass through the esophagus.
- Avoid Lying Down After Eating: Staying upright after meals can prevent regurgitation.
Homeopathy
Homeopathy offers remedies like:
- Carbo Veg: For bloating and indigestion.
- Lycopodium: For digestive discomfort and bloating.
- Nux Vomica: For heartburn and digestive issues.
It’s important to consult with a qualified homeopath before starting any treatment.
Ayurveda
Ayurvedic treatments for achalasia include:
- Herbal Remedies: Such as ginger, turmeric, and licorice to improve digestion.
- Panchakarma: A detoxification procedure to balance body energies.
- Dietary Changes: Emphasizing easily digestible foods and avoiding heavy, oily, and spicy foods.
Consulting with an Ayurvedic practitioner is essential to tailor treatments to individual needs.
Unani Medicine
Unani medicine approaches achalasia with:
- Herbal Remedies: Using herbs like fennel, mint, and black cumin to enhance digestion.
- Regimenal Therapy: Including massage and hydrotherapy to improve overall health.
As with other alternative therapies, it’s important to seek guidance from a qualified Unani practitioner.
Alternative Therapies
Various alternative therapies can support the management of achalasia, including:
- Acupuncture: May help relieve pain and improve esophageal function.
- Chiropractic Care: Focuses on improving nerve function and overall well-being.
- Mind-Body Techniques: Such as yoga and meditation to manage stress and improve digestion.
Foods
Diet plays a crucial role in managing achalasia. Recommended foods include:
- Soft foods: Yogurt, applesauce, mashed potatoes
- Liquids: Soups, smoothies
- Well-cooked vegetables and tender meats
Foods to avoid include:
- Spicy foods
- Citrus fruits
- Carbonated beverages
- Hard-to-swallow foods like dry bread and tough meat
Prevention
There is no known way to prevent achalasia, but early diagnosis and treatment can prevent complications. Maintaining a healthy lifestyle and seeking medical attention for persistent gastrointestinal symptoms can help manage the condition effectively.
Complications
Untreated achalasia can lead to several complications, including:
- Esophageal dilation: Widening of the esophagus
- Esophagitis: Inflammation of the esophagus
- Aspiration pneumonia: Due to food and liquids entering the lungs
- Esophageal cancer: Increased risk due to chronic irritation,a rare complication.
Emergency
In some cases, achalasia can lead to emergency situations, such as severe chest pain, difficulty breathing, or significant weight loss. Immediate medical attention is necessary in these cases.
Specialists to Visit
If you suspect you have achalasia, you should consult:
- Gastroenterologist: A specialist in digestive disorders.
- Surgeon: For surgical interventions if needed.
- Nutritionist: To help manage dietary changes.
Outlook
Living with Achalasia Cardia
Achalasia cardia, while disruptive, can be effectively managed with various treatment approaches. With proper diagnosis and treatment, individuals with achalasia can experience significant improvement in their symptoms and overall well-being.
Achalasia varies depending on the severity of the condition and the effectiveness of treatment. With proper management, many people can lead relatively normal lives, although ongoing monitoring may be necessary.
Achalasia is a complex condition, but with the right knowledge and treatment, it can be managed effectively. Whether you’re dealing with achalasia yourself or supporting a loved one, understanding the condition is the first step towards finding relief and improving quality of life.
REFERENCES
- Vaezi MF, Pandolfino JE, Vela MF. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol. 2013;108(8):1238-1249.
- Boeckxstaens GE, Zaninotto G, Richter JE. Achalasia. Lancet. 2014;383(9911):83-93.
- Eckardt AJ, Eckardt VF. Current clinical approach to achalasia. World J Gastroenterol. 2009;15(32):3969-3975.
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160-174.
- Patel DA, Naik RD, Slaughter JC, et al. Weight loss in achalasia: a model for the Cachexia Index. Dis Esophagus. 2018;31(9)
