A Vaginal discharge is a natural and essential component of female reproductive health. It’s a fluid produced by the glands in the cervix and vagina, and it plays a crucial role in maintaining a healthy vaginal environment. The vagina is a self-cleaning organ, and discharge is its natural way of flushing out dead cells, bacteria, and other debris. This discharge helps to prevent infections and keeps the vaginal tissues moist and healthy. The amount, color, and consistency of discharge can vary throughout the menstrual cycle, influenced by hormonal fluctuations and sexual activity. While most discharge is normal, certain changes can indicate underlying issues. Understanding these variations is vital for recognizing potential problems and seeking appropriate medical attention.
Types of Vaginal Discharge
There are two main categories of vaginal discharge:
Types
Physiological Discharge
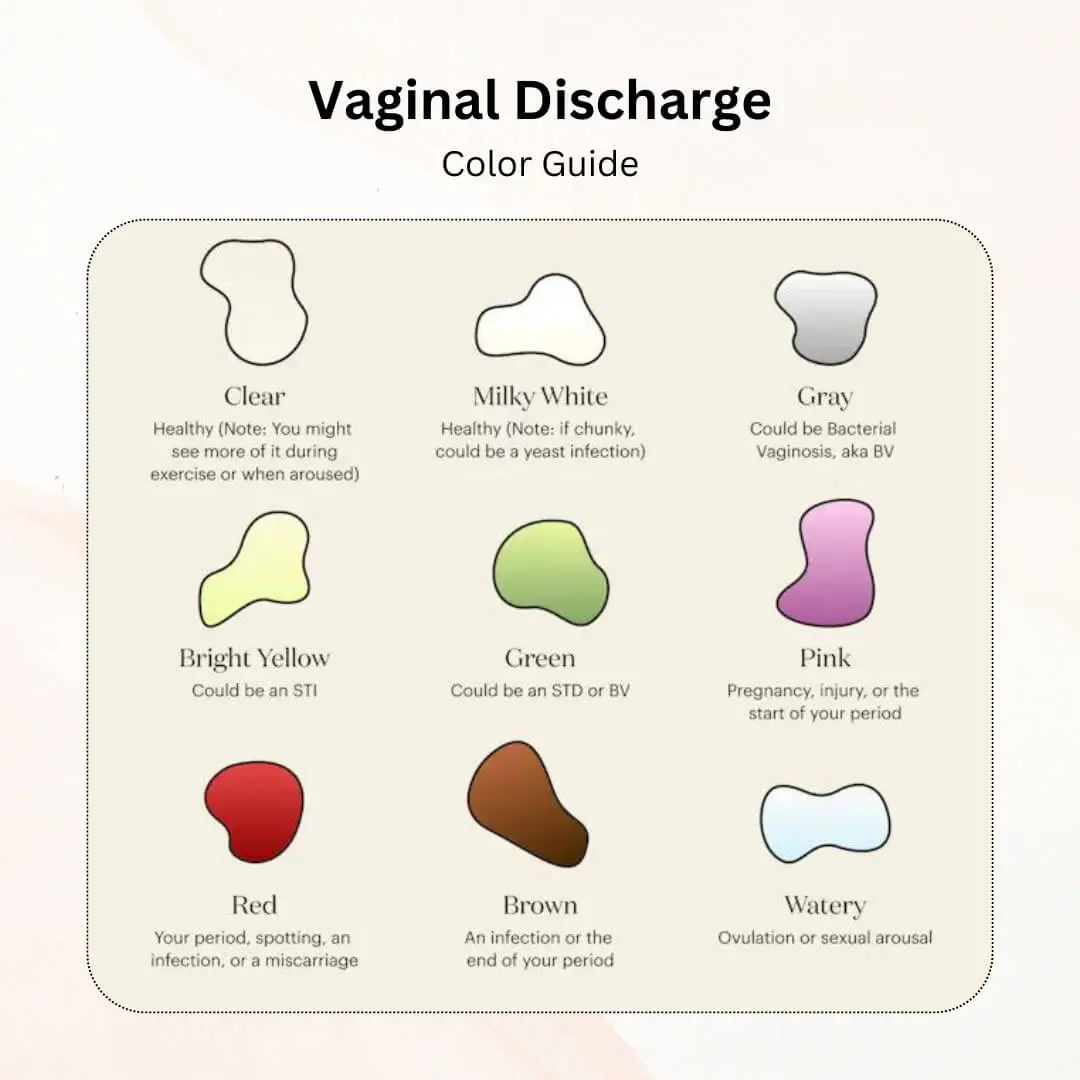
Physiological discharge is considered normal and can vary in consistency and color:
- Clear and Stretchy: Typically observed during ovulation.
- White and Creamy: Common in the early part of the menstrual cycle.
- Thin and Watery: May occur at different times of the cycle, especially after exercise.
Pathological Discharge
Pathological discharge indicates an underlying condition and is often accompanied by other symptoms such as itching, burning, or odor:
Infective – Sexually Transmitted
- Discharge is often green, yellow, or frothy and has a strong, unpleasant odor, fishy odor and associated with itching
- Mainly caused by Trichomonas vaginalis, Chlamydia trachomatis and Neisseria Gonorrhea
Infective – Non Sexually Transmitted
- Discharge is White and Clumpy: Resembles cottage cheese, curdy white often indicative of a yeast infection (candidiasis).
- Discharge is Greyish: Typically associated with bacterial vaginosis.
Non Infective Discharge
- Discharge is Brown or Bloody: May occur due to irregular menstrual cycles, cervical polyps, foreign body, fistulas and in genital tract malignancies
- Atrophic Vaginitis Discharge: This discharge is typically scanty and watery due to decreased estrogen levels, particularly after menopause.
Symptoms
Normal vaginal discharge typically doesn’t cause any discomfort or other symptoms. However, abnormal discharge might be accompanied by the following:
- Itching or burning sensation around the vagina or vulva
- Pain during intercourse
- Pain or burning during urination
- Redness or swelling of the vulva
- Strong, unpleasant odor, fishy odor.
If you experience any of these symptoms along with abnormal discharge, it’s crucial to consult a healthcare professional for diagnosis and treatment.
Causes
The causes of vaginal discharge can be broadly categorized into infectious and non-infectious:
Infectious Causes
Non Sexually Transmitted
- Bacterial Vaginosis: An imbalance of naturally occurring bacterial flora.
- Yeast Infections (Candidiasis): Overgrowth of Candida species.
Sexually Transmitted – Including gonorrhea, chlamydia, trichomoniasis, and herpes.
Non-Infectious Causes
- Hormonal Changes: During pregnancy, menopause, or the menstrual cycle.
- Ovulation: Around ovulation, discharge becomes clear, stretchy, and egg-white-like, facilitating sperm movement
- Medications: Antibiotics, birth control pills, and steroids can alter vaginal flora.
- Douching: Douching disrupts the natural balance of bacteria in the vagina, increasing the risk of infections and altered discharge.
- Sexual Arousal: Discharge increases during sexual arousal to lubricate the vagina.
- Pregnancy: During pregnancy, discharge increases in volume and becomes white and milky due to elevated estrogen levels.
- Foreign Bodies: Such as retained tampons or contraceptive devices.
- Allergic Reactions: To soaps, detergents, or douches.
Risks
Risk factors for developing abnormal vaginal discharge include:
- Multiple sexual partners or new sexual partner.
- Poor hygiene practices.
- Douching, which disrupts the natural vaginal flora.
- Uncontrolled diabetes.
- Use of scented personal care products.
Diagnosis
Diagnosis of abnormal vaginal discharge involves:
- Medical History : Detailed sexual history, symptoms duration, and associated factors.
- Physical Examination: Inspection of the vulva and vagina.
- Laboratory Test‘s:
- Vaginal swabs for microscopy, culture, and sensitivity.
- Pap smear test (Papanicolaou test)
- pH testing.
- Nucleic acid amplification tests (NAAT) for STIs.
Treatment
Treatment for vaginal discharge depends on the underlying cause:
- Normal Discharge: No treatment is necessary for normal vaginal discharge.
- Yeast Infection: Antifungal creams, suppositories, or tablets are typically prescribed to treat yeast infections.
- Bacterial Vaginosis: Antibiotics are usually prescribed to restore the balance of healthy bacteria in the vagina.
- Trichomoniasis: Antibiotics are prescribed for both you and your sexual partner(s) to eradicate the infection.
- STI Treatment: The specific treatment for STIs varies depending on the type of infection. It often involves antibiotics or other medications.
- Antiviral Drugs: For viral infections such as herpes.
- Atrophic Vaginitis: Estrogen creams, suppositories, or tablets can help replenish estrogen levels and improve vaginal lubrication.
In Children
Vaginal discharge in prepubescent girls is relatively uncommon. However, it can occur due to:
- Foreign Objects: Young children might insert small objects into the vagina, leading to irritation and discharge.
- Vulvovaginitis: This is an inflammation of the vulva and vagina, often caused by irritants like bubble bath, soap, or tight-fitting clothing.
- Pinworms: These tiny intestinal parasites can migrate to the vagina, causing itching and discharge.
If you notice vaginal discharge in your daughter, consult a paediatrician for diagnosis and treatment.
In Teens
Teens are more susceptible to vaginal discharge due to hormonal fluctuations associated with puberty. Normal discharge patterns might establish during this time. However, they should be aware of potential signs of abnormal discharge and underlying conditions like:
- Yeast Infections: Yeast infections are common among teens due to hormonal changes and antibiotic use.
- Bacterial Vaginosis: Similar to adults, bacterial imbalances can also occur in teens.
- STIs: Sexually active teens are at risk for contracting STIs, which can manifest as abnormal discharge.
In Adults
In adult women, the causes can be more varied:
- Hormonal contraceptives.
- Pregnancy.
- Perimenopause and menopause. Regular gynaecological check-ups are recommended for early detection and treatment.
In Pregnancy
During pregnancy, vaginal discharge increases significantly due to elevated estrogen levels. This discharge is typically:
- Clear or milky white
- Odorless Thin or slightly sticky discharge is seen normally.
- Increased normal discharge (leukorrhea).
Higher susceptibility to infections. Regular prenatal care includes screening and treatment for infections to prevent complications.
Homeopathy, Ayurveda, Unani Medicine, and Alternative Therapies
Complementary and alternative medicine (CAM) therapies like homeopathy, Ayurveda, Unani medicine, and certain alternative therapies might be explored for vaginal discharge concerns. However, it’s essential to approach these options with caution:
- Limited Scientific Evidence: There is limited scientific evidence to support the effectiveness of these therapies for treating vaginal discharge.
- Potential Risks: Some CAM therapies might have side effects or interact with medications you’re taking.
- Regulation: Regulation of CAM therapies can vary, so it’s crucial to choose a qualified practitioner who uses safe and effective methods.
Important Note: It’s highly recommended to consult a healthcare professional before using any CAM therapy for vaginal discharge. They can help you weigh the potential benefits and risks and ensure these therapies don’t interfere with any conventional treatments you might be receiving.
Homeopathy
Homeopathic remedies are tailored to individual symptoms and may include:
- Sepia: For white, yellow, or greenish discharge.
- Pulsatilla: For thick, creamy discharge.
- Kreosotum: For offensive-smelling discharge.
Ayurveda
Ayurvedic treatments focus on balancing the body’s doshas and may include:
- Triphala: A blend of three fruits for cleansing and detoxification.
- Aloe Vera: Used both topically and internally.
- Yoni Prakshalan: Herbal vaginal wash.
Unani Medicine
Unani medicine uses natural herbs and compounds for treatment, such as:
- Shatavari: To balance female hormones.
- Majoon Supari Pak: For general reproductive health.
- Arq Gulab: As a soothing wash.
Alternative Therapies
Alternative therapies that may support vaginal health include:
- Acupuncture: To balance body energies.
- Herbal Supplements: Such as Echinacea and goldenseal for immune support.
- Aromatherapy: Using essential oils like lavender and chamomile for relaxation and symptom relief.
Natural Remedies
For mild cases of discomfort associated with normal discharge, some natural remedies might offer relief:
- Sitz Baths: Soaking in a warm sitz bath with plain water or diluted vinegar can provide soothing relief for itching and burning.
- Probiotics: Taking probiotic supplements or consuming yogurt with live cultures might help restore the balance of healthy bacteria in the vagina.
- Loose-fitting Cotton Underwear: Wearing breathable cotton underwear helps keep the vaginal area cool and dry.
- Gentle Cleansing: Avoid harsh soaps and douches, which can disrupt the natural vaginal flora. Use a gentle, fragrance-free cleanser specifically formulated for the vulva.
Important Note: It’s crucial to consult a healthcare professional before using any natural remedies, especially if you have a confirmed infection or underlying medical condition.
Foods
Diet can indirectly influence vaginal health. While no specific foods directly cause vaginal discharge, certain dietary choices might contribute to a healthy vaginal environment:
- Probiotics: Yogurt with live and active cultures or probiotic supplements can help maintain a healthy balance of good bacteria in the vagina.
- Cranberries: Cranberries contain compounds that may help prevent UTIs, which can sometimes mimic vaginal discharge symptoms.
- Fruits and Vegetables: A diet rich in fruits and vegetables provides essential vitamins and nutrients that support overall health, including vaginal health.
It’s important to note that there are no miracle foods for treating abnormal discharge. However, maintaining a healthy diet can contribute to overall well-being and potentially reduce the risk of infections.
Prevention
Several steps can be taken to prevent abnormal vaginal discharge and maintain healthy vaginal flora:
- Practice good hygiene: Wash the vulva daily with warm water and a gentle, fragrance-free cleanser. Avoid douching, which disrupts the natural balance of bacteria.
- Wipe from front to back: This helps prevent bacteria from entering the vagina from the anus.
- Wear cotton underwear: Opt for breathable, loose-fitting cotton underwear to allow for air circulation and prevent moisture buildup.
- Practice safe sex: Consistent and correct condom use can help prevent STIs that can cause abnormal discharge.
- Avoid harsh soaps and detergents: These can irritate the vulva and vagina, potentially leading to discharge.
- Maintain a healthy diet: As mentioned earlier, a balanced diet rich in fruits, vegetables, and probiotics can promote overall health and potentially reduce the risk of infections.
By incorporating these preventive measures into your routine, you can significantly reduce the risk of developing abnormal vaginal discharge.
Complications
Ignoring abnormal vaginal discharge can lead to various complications, including:
- Spreading Infections: Untreated infections can spread to the uterus and fallopian tubes, potentially leading to pelvic inflammatory disease (PID). PID can increase the risk of infertility and ectopic pregnancy.
- Increased Risk of STIs: Changes in vaginal flora due to abnormal discharge can make you more susceptible to contracting STIs.
- Cervical Cancer: While not directly caused by vaginal discharge itself, HPV, a sexually transmitted virus that can cause abnormal discharge, is also a risk factor for cervical cancer. Regular Pap smears are crucial for early detection and prevention.
- Emotional Distress: Concerns about abnormal discharge can cause stress and anxiety.
Early diagnosis and treatment of abnormal discharge are essential to prevent these potential complications and maintain overall reproductive health.
Emergency
If you experience any of the following symptoms along with vaginal discharge, seek immediate medical attention:
- Severe pain in the lower abdomen or pelvis
- High fever
- Heavy bleeding
- Foul-smelling discharge
- Signs of an allergic reaction, such as difficulty breathing or swelling
These symptoms could indicate a serious underlying condition requiring prompt medical evaluation and treatment.
Specialist to Visit
For concerns related to vaginal discharge, you should consult a healthcare professional. Depending on your specific situation, you might see:
- Obstetrician-Gynaecologist (OB-GYN): This is a specialist in women’s reproductive health and is often the primary healthcare provider for women with vaginal discharge concerns.
- Family Physician or Internal Medicine Doctor: These primary care doctors can diagnose and treat common vaginal discharge issues.
- Paediatrician: If you have concerns about vaginal discharge in your daughter, consult a paediatrician.
Don’t hesitate to discuss any questions or concerns you have about vaginal discharge with your healthcare professional. They can provide personalized guidance and ensure you receive the appropriate diagnosis and treatment.
Outlook
Most cases of abnormal vaginal discharge can be treated effectively with appropriate medical intervention. The prognosis is generally good if the underlying cause is identified and managed timely.
REFERENCES
- N Nugent, MR Sheldon, KV Hague. Randomized controlled trial of metronidazole and clotrimazole ovules for the treatment of bacterial vaginosis. BJOG: An International Journal of Obstetrics and Gynaecology 1991;98(4):335-339. doi: 10.1111/j.1471-0328.1991.tb02223.x
- S Sobel. Vaginitis and vulvovaginitis. Epidemiology 2006;17(2 Suppl):S10-S17. doi: 10.1093/epidem/cdl016
- S Bradshaw, PE Hill, GHD Holmes. Cause-specific diagnosis of abnormal vaginal discharge in women attending a clinic for sexually transmitted diseases. British Journal of Venereal Diseases 1996;72(2):119-123. doi: 10.1136/bjdv.72.2.119
- A Wojnarowska, M Sobel. Diagnosis and treatment of vulvovaginal candidiasis. Clinical Infectious Diseases 2003;37(1):S170-S177. doi: 10.1086/375222
- Workowski KA, Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2021. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports 2021;70(12):1-190. doi: 10.1558/mmwr.rr7012a1
